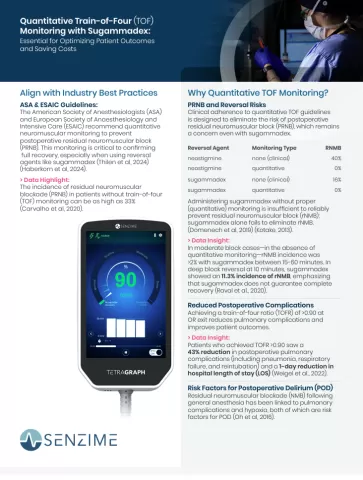
ASA and ESAIC recommend quantitative neuromuscular monitoring to prevent postoperative residual neuromuscular block. This monitoring is critical to confirming full recovery, especially when using reversal agents like sugammadex. (Thilen et al, 2024) (Haberkorn et al, 2024)
Your Dynamic Duo: Sugammadex & Quantitative TOF Monitor with Dr. Ross Renew (U.S) & Dr. Grant Rodney (U.K.)
On-demand webinar
Quantitative TOF monitoring combined with sugammadex delivers powerful advantages in patient safety, drug savings, and operational efficiency.
70% reduction
Ref: Thilen et al., 2024
$370,000 with TOF-based dosing
Ref: Haberkorn et al., 2024
43% lower rate with TOFR >0.90
Ref: Weigel et al., 2022
1-day shorter stay
Ref: Weigel et al., 2022
Bringing the next-generation TetraGraph into our community hospital has transformed how we manage neuromuscular block.
It has improved patient safety, standardized our practices, and reduced our annual drug spend by more than $100,000.
- Dr. Aaron Persinger
Anesthesiologist, Boulder Valley Anesthesiology Medical Director, UCHealth Broomfield Anesthesiology Medical Director, Pre-Anesthesia Testing Clinic, UCHealth Broomfield

Clinical adherence to quantitative TOF guidelines is designed to eliminate the risk of postoperative residual neuromuscular block, which remains a concern even with sugammadex.
Administering sugammadex without proper (quantitative) monitoring is insufficient to reliably prevent residual neuromuscular block; sugammadex alone fails to eliminate RNMB.
- Neostigmine without monitoring: 40% RNMB
- Neostigmine with monitoring: 0% RNMB
- Sugammadex without monitoring: 16% RNMB
- Sugammadex with monitoring: 0% RNMB
(Domenech et al, 2019) (Kotake, 2013)

Achieving a train-of-four ratio (TOFR) of more than 0.90 at OR exit reduces pulmonary complications and improves patient outcomes.
Patients who achieved TOFR >0.90 saw a 43% reduction in postoperative pulmonary complications (including pneumonia, respiratory failure, and reintubation) and a 1-day reduction in hospital length of stay (LOS). (Weigel et al., 2022)


- Reduction in drug wastage
Quantitative TOF monintoring enables precise sugammadex dosing. - Decreased PACU time
Efficient reversal with TOF monitoring shortens PACU discharge times, optimizing turnover and resource allocation. - Increased efficiency
Cost savings are achievable when the use of sugammadex is selectively guided by quantitative monitoring (Thilen et al., 2024).
Quantitative TOF monitoring allows anesthesiologists to tailor sugammadex dosing accurately, minimizing under- or overdosing risks.
In a study of 97 patients, 87% required less sugammadex than the recommended dose, and 13% required more (Bowdle et al., 2023).

Guided by quantitative monitoring, selecting the appropriate reversal agent (neostigmine or sugammadex) can significantly cut costs.
A study involving 189 patients revealed that reversing all patients with sugammadex would have resulted in a total cost of USD 19,312 (USD 102 per patient), which is 70% higher than the cost achieved through optimized selective use.

Aliquoting sugammadex into smaller doses, combined with quantitative TOF, further reduces medication waste and costs.
An institution projected annual savings of nearly $370,000 by aliquoting sugammadex and confirming adequate recovery without sugammadex in 20% of cases (Haberkorn et al, 2024).

Despite its efficacy, sugammadex demonstrates variability in response which underpins the need for quantitative train-of-four (TOF) monitoring.
- Dr. Grant Rodney, Consultant Anaesthetist, Dundee, NHS Tayside, Scotland

Powered by the latest, most accurate EMG technology, TetraGraph elevates the operating room experience with intelligent design and unmatched precision. It supports you throughout an entire case and helps to streamline your workflow.
TetraGraph is the monitor of choice for thousands of clinicians worldwide.
Get your info sheet on how to use quantitative TOF monitoring in combination with sugammadex.
We are here to guide you. Contact us to learn more why you need quantitative TOF monitoring even when using sugammadex.
- Thilen SR, et al. “Management of Muscle Relaxation with Rocuronium and Reversal with Neostigmine or Sugammadex Guided by Quantitative Neuromuscular Monitoring.” Anesthesia & Analgesia, 2024; 139(3):536-544 (Management_of_Muscle_Re…).
- Shorten GD, Merk H, Sieber T. Perioperative train-of-four monitoring and residual curarization. Can J Anaesth. 1995 Aug;42(8):711-5. doi: 10.1007/BF03012670. PMID:7586111.
- Haberkorn S, Faulk DJ, et al. “Quantitative Monitoring Maximizes Cost-Saving Strategies When Antagonizing Neuromuscular Block with Sugammadex.” Cureus, 2024; 16(9): e68551. DOI: 10.7759/cureus.68551(2024 - Haberkorn S, Fau…).
- Domenech, G., Kampel, M.A., García Guzzo, M.E. et al. Usefulness of intra-operative neuromuscular blockade monitoring and reversal agents for postoperative residual neuromuscular blockade: a retrospective observational study. BMC Anesthesiol 19, 2019.
- Kotake, Y. Reversal with sugammadex in the absence of monitoring did not preclude residual neuromuscular block. Anesth. Analg, 2013.
- Raval AD, Uyei J, Karabis A, Bash LD, Brull SJ. “Incidence of residual neuromuscular block and use of neuromuscular blocking agents with or without antagonists: A systematic review and meta-analysis of randomized controlled trials.” Journal of Clinical Anesthesia, 2020; 64:109818. https://doi.org/10.1016/j.jclinane.2020.109818.
- Weigel WA, Williams BL, Hanson NA, et al. “Quantitative Neuromuscular Monitoring in Clinical Practice: A Professional Practice Change Initiative.” Anesthesiology, 2022; 136(6):901-915. DOI: 10.1097/ALN.0000000000004174.
- T. Andrew Bowdle, Kishanee J. Haththotuwegama, Srdjan Jelacic, Sharon T. Nguyen, Kei Togashi, Kelly E. Michaelsen; A Dose-finding Study of Sugammadex for Reversal of Rocuronium in Cardiac Surgery Patients and Postoperative Monitoring for Recurrent Paralysis. Anesthesiology 2023; 139:6–15 doi: https://doi.org/10.1097/ALN.0000000000004578
- Oh CS, Rhee KY, Yoon TG, Woo NS, Hong SW, Kim SH. Postoperative Delirium in Elderly Patients Undergoing Hip Fracture Surgery in the Sugammadex Era: A Retrospective Study. Biomed Res Int. 2016;2016:1054597. doi: 10.1155/2016/1054597. Epub 2016 Feb 22. PMID: 26998480; PMCID: PMC4779812
- Carvalho H, et al.: Forty years of neuromuscular monitoring and postoperative residual curarisation: a meta-analysis and evaluation of confidence in network meta-analysis. Br J Anaesth. 2020 Oct;125(4):466-482.
- Bowdle TA, Haththotuwegama KJ, Jelacic S, Nguyen ST, Togashi K, Michaelsen KE. A Dose-finding Study of Sugammadex for Reversal of Rocuronium in Cardiac Surgery Patients and Postoperative Monitoring for Recurrent Paralysis. Anesthesiology. 2023 Jul 1;139(1):6-15. doi: 10.1097/ALN.0000000000004578. PMID: 37027807.
