Why protocols matter in the healthcare setting
June 17, 2025
By Amanda Kingery, RN, BSN, CNRN, Clinical & Medical Affairs Coordinator at Senzime
Protocols are fundamental to delivering safe, consistent, and effective healthcare. They provide clear, evidence-based guidelines that help providers navigate complex clinical environments, reduce errors, and uphold best practices. Think of protocols as a form of legal and professional protection, supporting the patient and the provider. Without clearly defined standards, even the most skilled clinicians may face an increased risk of miscommunication, inefficiency, and/or clinical error.
Whether in hospitals, ambulatory surgery centers, or clinics, protocols play a critical role in ensuring patient safety and operational consistency.
Here are five key reasons why protocols are essential in the healthcare setting:

Protocols grounded in evidence-based research help healthcare teams deliver the highest standards of care. They are designed to minimize variability, prevent errors, and ensure that patient safety remains the top priority across all settings.
With guidelines in place, providers can make faster, safer decisions even under pressure.

Standardized protocols promote seamless communication and task delegation among multidisciplinary teams.
By clearly defining roles, responsibilities, and workflows, protocols ensure everyone is aligned—resulting in smoother transitions of care, reduced duplication, and improved clinical outcomes.

Most protocols stem from regulatory requirements or advancements communicated by governing bodies. When institutions adopt and adhere to these guidelines, they not only remain compliant with laws and accreditation standards but also reduce legal risk.
In the event of a malpractice claim, documented adherence to a protocol can be a powerful defense that demonstrates due diligence and clinical integrity.

Protocols are essential for onboarding and continuing education. They provide new staff with a clear understanding of clinical expectations and offer experienced providers a reference point as new guidelines emerge.
By centralizing knowledge and expectations, healthcare organizations can quickly adapt to new evidence, technologies, or best practices while maintaining system-wide consistency.

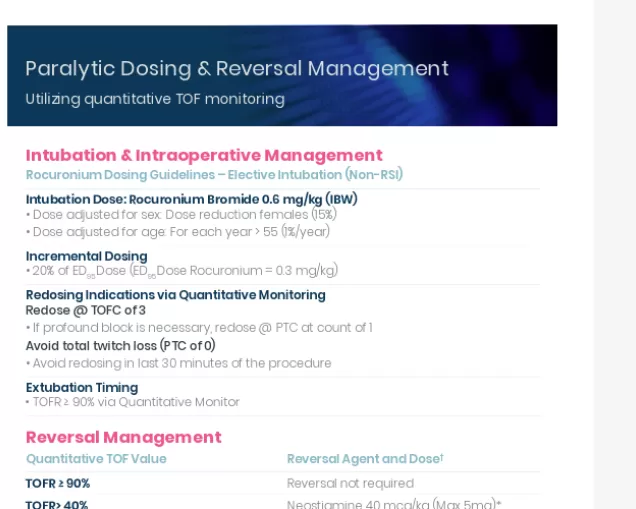
One impactful area for protocol development is the use of quantitative train-of-four (TOF) monitoring during paralytic management. Devices like Senzime’s EMG-based TetraGraph® enable clinicians to precisely monitor and reverse neuromuscular block, reducing the risk of residual paralysis.
Developing and following a protocol for quantitative monitoring helps care teams:
- Confirm adequate recovery before extubation
- Avoid under- or over-dosing of reversal agents
- Improve patient safety and outcomes
- Align with ASA, ESAIC, and other society guidelines
- Reduce variation in patient outcomes across providers and settings
By integrating a standardized, evidence-based approach to neuromuscular monitoring, healthcare systems can strengthen both safety and efficiency.
Protocols in healthcare are not about limiting professional judgment—they provide a trusted foundation that supports safer decisions, enhances collaboration, and ensures consistent, high-quality care.
This protocol is based on on ASA’s practice guidelines.
Amanda Kingery, RN, BSN, CNRN, Clinical & Medical Affairs Coordinator at Senzime
If you have any further questions or require additional information, feel free to contact me and my colleagues.

