Sept 30, 2024
By Jamie Dupont RN, BSN, CCRN - Clinical Product Specialist at Senzime

Accurate management of neuromuscular block during anesthesia is crucial for patient safety. However, the implementation of quantitative TOF monitoring devices can be challenging due to various barriers.
In this blog post, we will explore the basics of TOF monitoring based on electromyography (EMG), identify common barriers to its implementation, discuss strategies for overcoming these obstacles, navigate equipment and technological challenges, and explore how to cultivate a culture of change in anesthesia practice.
Quantitative train-of-four (TOF) assessment is essential in anesthesia to manage neuromuscular block during surgical procedures. At its core, the TetraGraph monitor utilizes EMG to evaluate the action potential at the neuromuscular junction in response to a series of four nerve stimulations. This sequence of stimuli is critical for assessing the depth of neuromuscular block and determining the adequacy of muscle relaxation and ensuring proper reversal. When applying these consecutive electrical pulses, TetraGraph calculates fade between T4 and T1, quantifying the data into a TOF ratio percentage to assure adequate block and recovery.
This method stands out for its ability to deliver real-time feedback on neuromuscular function, enabling anesthesia clinicians to tailor their use of neuromuscular blocking agents (NMBAs) with greater precision. The goal is to achieve a balance that ensures sufficient muscle relaxation for the procedure while minimizing the risk of postoperative residual neuromuscular block (rNMB), which can lead to complications such as impaired respiratory function and inadequate airway recovery.
Effective neuromuscular monitoring requires an understanding of both the technical aspects of the equipment and the physiological implications of the readings. It involves not only the accurate placement of electrodes and the interpretation of the TOF ratio but also an appreciation of how various factors, including the choice of NMBA and the patient’s condition, can influence neuromuscular transmission (NMT) and recovery. By mastering EMG TOF monitoring, anesthesia clinicians can enhance patient safety and outcomes, making it a critical component of modern anesthesia management.
Implementing quantitative TOF monitoring into clinical practice encounters several hurdles that can impact its widespread adoption. A significant obstacle is anesthesia clinicians' familiarity and comfort level with the novel technology. Continued education and technical proficiency are key components to success. Furthermore, the integration of quantitative TOF monitoring faces logistical challenges, including the procurement and access to specialized equipment. The availability of such equipment may be inconsistent across different healthcare settings, ranging from well-equipped tertiary care centers to resource-constrained environments. This disparity affects the uniformity in the application of neuromuscular monitoring techniques. Placing a quantitative TOF monitor in each anesthetizing location has been identified as a key contributing factor to successful implementation and adoption (Weigel et al, 2022).
Interpreting quantitative TOF monitoring results also presents a barrier. The accurate analysis of TOF ratios requires a nuanced understanding of neuromuscular physiology and the pharmacodynamics of neuromuscular blocking agents. “Clinicians who have little exposure to objective monitors are often unaware of the subtle yet important differences between data obtained from quantitative monitors and the limited (and erroneous) information generated by subjective evaluation using PNS or clinical signs of recovery” (Naguib et al., 2018). Misinterpretation of these results can lead to suboptimal patient management, such as inadequate neuromuscular block or prolonged recovery times. Signal strength and transparent EMG waveforms that are displayed on the TetraGraph provide clinician confidence when interpreting and understanding the accuracy of EMG readings. A signal strength of at least 5mV (measured at T1 prior to paralysis) indicates good placement on the ulnar nerve despite possible anatomical variability from patient to patient.
Resistance to change within anesthesia practice further complicates the adoption of TOF monitoring. The process of unlearning or “de-implementation” of outdated practices such as qualitative monitoring is a challenge for clinicians (Naguib et al., 2018). Established routines and preferences for subjective assessment methods over quantitative tools can inhibit the transition to more advanced monitoring techniques. Overcoming these barriers necessitates targeted efforts to educate and engage anesthesia clinicians on the benefits and practical aspects of TOF monitoring, aiming to elevate the standard of care in anesthesia management.
Bridging the educational divide in the realm of TOF monitoring requires innovative and comprehensive strategies. A pivotal approach is the development and deployment of specialized training modules that are integrated into both initial anesthesia training programs and ongoing professional development courses. These modules should be designed to cover the full spectrum of TOF monitoring, from the basic principles and technical operation of the equipment to the intricate details of interpreting the data in the context of patient management.
Interactive workshops and simulation-based training sessions can play a critical role in enhancing the hands-on skills of anesthesia clinicians. Through these interactive sessions, participants can gain practical experience in placing electrodes correctly, operating the monitoring equipment, and making informed clinical decisions based on TOF readings. These workshops also provide a platform for anesthesia clinicians to discuss case scenarios and share best practices, fostering a collaborative learning environment.
Identifying departmental super users and providing continued support and education can further supplement these educational efforts. Pairing less experienced clinicians with seasoned experts in neuromuscular monitoring allows for the transfer of knowledge and skills that are not always captured in formal training programs. This one-on-one guidance can help new clinicians become more comfortable and proficient with quantitative TOF monitoring techniques.
Leveraging online learning resources, including webinars, instructional videos, and forums, can also bridge the gap in knowledge and skills. These resources offer the flexibility for anesthesia clinicians to learn at their own pace and revisit complex topics as needed, ensuring a thorough understanding of quantitative TOF monitoring principles and practices.
By embracing a multifaceted approach to education, the anesthesia clinicians can overcome the barriers associated with implementing quantitative TOF monitoring, ultimately enhancing patient care and safety.
Addressing the hurdles associated with equipment and technology is a crucial step toward the effective implementation of EMG train-of-four (TOF) monitoring. The initial challenge lies in securing the acquisition of high-quality, reliable electromyography (EMG) devices such as TetraGraph. This requires careful selection to ensure compatibility with existing systems and ease of use for clinicians.
Another layer of complexity is introduced by the rapid evolution of neuromuscular monitoring technologies. Keeping abreast of the latest advancements and integrating them into clinical practice demands ongoing education and training for anesthesia clinicians. It also necessitates regular updates to equipment, which may include software upgrades or the acquisition of new devices offering enhanced functionalities.
To successfully navigate these challenges, healthcare facilities must establish strong relationships with manufacturers and suppliers, ensuring prompt support and access to training resources. Additionally, developing a structured process for the regular review and assessment of monitoring equipment can help identify potential issues before they impact clinical outcomes. Collaboration among anesthesia teams to share insights and solutions related to equipment use and troubleshooting can further mitigate technological challenges, enabling a smoother integration of quantitative TOF monitoring into anesthesia practice.
Embedding a culture of change within anesthesia teams is imperative for the fruitful adoption of quantitative TOF monitoring. Embracing change requires a willingness from all team members to question the status quo and explore innovative practices that advance patient care. A key component is the cultivation of an environment where continuous learning is valued and supported.
Another key component is collaboration. Open dialogue about the challenges and successes associated with TOF monitoring fosters a sense of community and collective responsibility among team members. By sharing experiences and solutions, the team can navigate the complexities of implementing this technology together, making the process less daunting and more achievable. The third key component is leadership support. Leaders play a crucial role in setting the tone for change, providing the necessary resources, and championing the benefits of quantitative TOF monitoring. Their endorsement underscores the value placed on advancing patient safety and the quality of anesthesia care.
Ultimately, cultivating a culture of change involves a holistic approach that incorporates education, collaboration, and leadership. Through these concerted efforts, anesthesia practices can seamlessly integrate quantitative TOF monitoring, setting a new standard for patient care and safety in the surgical setting.
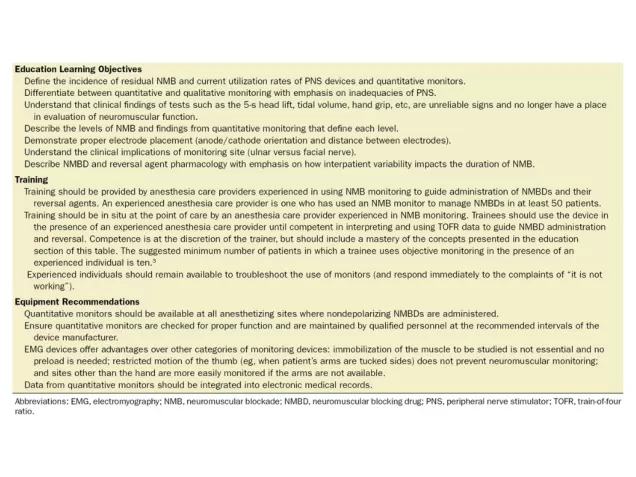
Table 3. Adopted from Naguib et al, regarding the recommended education, training and neuromuscular block monitoring equipment.
Senzime is committed to providing the most comprehensive precision-based EMG technology, safeguarding every patient's journey. We offer best-in-class implementation strategies, providing expert in-person education and ongoing support. We highly value our hospital partnerships across the globe and invite you to reach out for more information on elevating your anesthesia practice.
Together we can eliminate residual neuromuscular block and improve patient safety!
Wade A. Weigel, Barbara L. Williams, Neil A. Hanson, C. Craig Blackmore, Randy L. Johnson, Gary M. Nissen, Andrew B. James, Wyndam M. Strodtbeck; Quantitative Neuromuscular Monitoring in Clinical Practice: A Professional Practice Change Initiative. Anesthesiology 2022; 136:901–915 doi: https://doi.org/10.1097/ALN.0000000000004174
Naguib, Mohamed; Brull, Sorin J.; Kopman, Aaron F.; Hunter, Jennifer M.; Fülesdi, Béla; Arkes, Hal R.; Elstein, Arthur; Todd, Michael M.; Johnson, Ken B. Consensus Statement on Perioperative Use of Neuromuscular Monitoring Anesthesia & Analgesia127(1):71-80, July 2018. doi: 10.1213/ANE.0000000000002670
Jamie Dupont RN, BSN, CCRN - Clinical Product Specialist at Senzime
If you have any further questions or require additional information, feel free to contact me and my colleagues.

Feel free to get in touch to talk to a sales representative about latest technology advancements or request a complimentary demo.
