Upcoming guidelines pave the way for safer pediatric neuromuscular block management
June 12, 2025
By AnnaMaria Tahlén, Global Digital & Brand Marketing Manager

In this blog, we will discuss the need for monitoring in pediatric anesthesia and how the upcoming European guidelines could help drive safer anesthesia practice worldwide.
New pediatric-specific guidelines are on the horizon, recommending the use of quantitative neuromuscular monitoring during anesthesia in children. This announcement, made at the recent Euroanaesthesia 2025 congress in Lisbon, marks a significant step toward improving perioperative safety in pediatric patients.
The final guidelines are expected later this year and will be the first to specifically advocate for this practice in pediatrics.
Each year, approximately 10-12 million major pediatric surgeries worldwide involve the use of neuromuscular blocking agents (NMBAs). For the United States alone, it’s close to 3 million cases per year. NMBAs are commonly used to facilitate endotracheal intubation and optimize surgical conditions.
However, without proper monitoring, up to 40 percent of pediatric patients experience residual neuromuscular block (rNMB) during the postoperative period. This can lead to respiratory complications, airway obstruction, and delayed recovery. (1,2).
Despite the well-known risks of residual paralysis, pediatric anesthesia has historically relied on qualitative monitoring and often no monitoring at all, due to the lack of pediatric-specific sensors.
The good news is that electromyography (EMG)-based quantitative train-of-four (TOF) monitoring is now available and offers an accurate and reliable option for monitoring in pediatrics.
As part of the session Hot topics in ESAIC Guidelines (part II) at Euroanaesthesia 2025, Dr. Francis Veyckemans announced the development of new European guidelines focused on pediatric neuromuscular block (NMB) management.
Highlighting a clear need for pediatric-specific guidance, Dr. Francis Veyckemans pointed out that current practices lag behind adult standards—especially concerning the use of NMB monitoring. (3)
One of the most concerning practices in pediatric anesthesia today is the administration of sugammadex without a quantitative TOF monitor. Sugammadex is a selective relaxant-binding agent that encapsulates NMBA molecules, allowing rapid reversal of neuromuscular block.
However, without quantitative neuromuscular monitoring, studies have shown that 87 percent of patients may receive an excessive dose and 13 percent an insufficient dose, increasing the risk of recurarization or prolonged paralysis.(4)
Encouragingly, advancements in monitoring technology, especially EMG-based systems, are now making it more feasible to apply quantitative monitoring in infants and children. These innovations represent great potential for safer perioperative care.
The forthcoming guidelines are expected to align closely with adult standards while addressing pediatric-specific considerations. They will prioritize evidence-based recommendations and focus on areas in the need of further research. The guidelines are expected to be officially released later in 2025.
The adult neuromuscular monitoring guidelines were published in late 2022, nearly simultaneously by both the American Society of Anesthesiologists (ASA) and the European Society of Anesthesia and Intensive Care (ESAIC).
Since then, these guidelines have significantly raised awareness about the importance of neuromuscular monitoring and contributed to a broader adoption of quantitative techniques in clinical practice.
Can we expect a similar shift in pediatric anesthesia when the new guidelines are released? The hope—and expectation—is yes.
The upcoming pediatric guidelines have the potential to drive change in clinical practice, moving toward safer, evidence-based anesthesia care.
As we wait for their release, it’s time for hospitals, clinicians and equipment providers to prepare for this shift, to make sure every pediatric patient can benefit from the same standards increasingly seen in adult care.
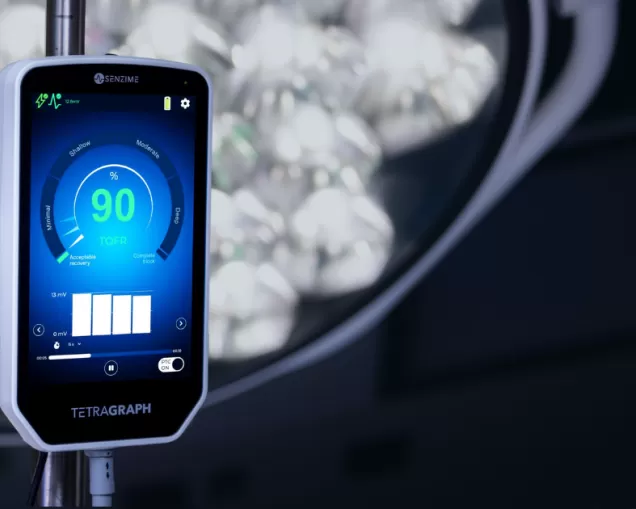
The next-generation TetraGraph® system, equipped with the soft and flexible TetraSens Pediatric sensor, delivers real-time and precise EMG-based assessment of neuromuscular function.
Unlike traditional acceleromyography (AMG) monitors, TetraGraph eliminates the need for free-moving muscles, making it ideal for pediatric patients, especially during tucked-arm laparoscopic and robotic surgical cases.
TetraSens Pediatric is an FDA-cleared EMG sensor with a separate and specific pediatric indication from one month old (defined as 28 days).
Contact our team to explore this solution or explore it at our pediatric page.
- New preliminary European guidelines for pediatric anesthesia will recommend quantitative neuromuscular monitoring to improve safety in children receiving neuromuscular blocking agents.
- Up to 40% of pediatric patients experience residual neuromuscular block (rNMB) postoperatively—posing serious risks when monitoring is absent or qualitative.
- TetraGraph, with its TetraSens Pediatric sensor, delivers an advanced EMG-based monitoring solution that positions clinicians to meet the upcoming pediatric guidelines with confidence.
AnnaMaria Tahlén, Global Digital & Brand Marketing Manager at Senzime
If you have any further questions or require additional information, feel free to contact me and my colleagues.

- Faulk DJ, Karlik JB, Strupp KM, Tran SM, Twite M, Brull SJ, Yaster M, Austin TM. The Incidence of Residual Neuromuscular Block in Pediatrics: A Prospective, Pragmatic, Multi-institutional Cohort Study. Cureus. 2024 Mar 18;16(3):e56408. doi: 10.7759/cureus.56408. PMID: 38638790; PMCID: PMC11024486.
- Engelhardt T, Virag K, Veyckemans F, Habre W.Airway Management in Paediatric Anaesthesia in Europe – Insights from APRICOT (Anaesthesia Practice in Children Observational Trial): A prospective multicentre observational study in 261 hospitals in Europe. Br J Anaesth 2018, 121; 66-75.
- Dr. Francis Veyckemans (Brussels, Belgium), May 26, ESAIC Guidelines (C) on muscle relaxation in anaesthetised children: indications, monitoring, and reversal, Hot topics in ESAIC Guidelines (part II), Euroanaesthesia 2025, Lisbon, Portugal.
- Bowdle TA, Haththotuwegama KJ, Jelacic S, Nguyen ST, Togashi K, Michaelsen KE. A Dose-finding Study of Sugammadex for Reversal of Rocuronium in Cardiac Surgery Patients and Postoperative Monitoring for Recurrent Paralysis. Anesthesiology. 2023 Jul 1;139(1):6-15. doi: 10.1097/ALN.0000000000004578. PMID: 37027807.
